Researchers at Indiana Center for Regenerative Medicine and Engineering at Indiana University School of Medicine are looking to a molecule to help wound healing in patients with diabetes.
Diabetes is a disease in which the body does not produce insulin, or when the body can no longer use that insulin properly. Insulin is a hormone made by the pancreas that allows the body to turn glucose, or sugar, into energy. If the body has difficulty metabolizing sugar, it can lead to high blood sugar levels.
Symptoms of symptoms of Type 1 or Type 2 diabetes include increased thirst and urination, increased hunger, fatigue, blurred vision, numbness or tingling in the feet or hands, unexplained weight loss, or sores that do not heal.
The sores that don’t heal can lead to what is known as a diabetic foot ulcer. The condition may cause patients to be hospitalized due to infection or other ulcer-related complications and may lead to amputation.
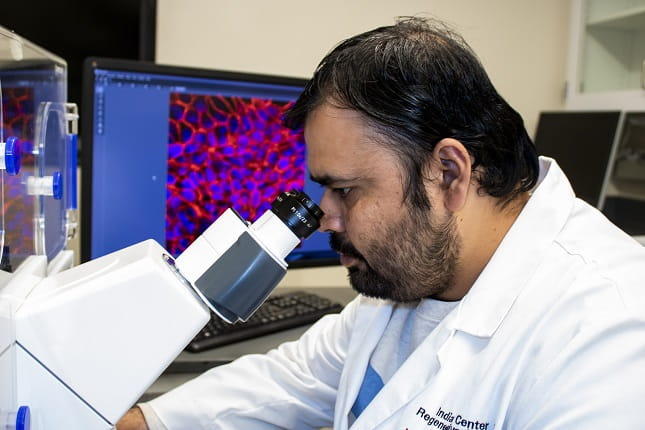
This is something that researchers at the Indiana Center for Regenerative Medicine and Engineering are looking to combat.
We sat down with Kanhaiya Singh, PhD, a postdoctoral fellow in Surgery and first author in a research study that identified a molecule that could be responsible for the cause of slow and improper healing in those who suffer from diabetes.
Can you summarize the main points of the study?
In patients with diabetes, there is a significant problem in the healing of their wounds. The defects that we see in these patients are that the cells necessary for wound healing don’t move to the wound site to close correctly.
This occurs due to a defect in a process called Epithelial-Mesenchymal transition (EMT). The other issue that we see is that the sprouting of new blood vessels, a process called angiogenesis, is not sufficient in these patients. Due to these two defects, diabetic wounds don’t close properly.
In our study, we looked into what regulators in this process can hinder diabetic wound healing. We found one target gene called Zeb1. In healthy individuals, this gene is responsible for the migration of the cells that help promote healing and the creation of new blood vessels. In norm glycemic condition, Zeb1 deficiency cause death of blood vessel forming endothelial cells. However, during hyperglycemia, Zeb1 loses its ability to bind to its partners. Hence, under diabetic conditions, elevated Zeb1 levels may contribute to the commonly noted persistent inflammatory response.
Why is it important to have vascularization for wound healing?
Newly formed granulation tissue needs more oxygen and nutrients because cells are actively dividing and migrating at the wound site. Hence, it needs proper vascularization so that newly formed blood vessels help the cells present at the wound site to receive proper nutrition and oxygen supply.
What were the key findings in the research?
This work recognizes Zeb1 as a significant mechanistic hub across epithelial and endothelial cells on the wound tissue microenvironment. In both of these cellular compartments, Zeb1 is responsive to the glycemic status of the injury microenvironment. Both low and excessive Zeb1 levels are pathogenic, pointing toward the critical need to tune Zeb1 levels to intermediary levels optimal for wound repair.
How will this research help patients?
From a therapeutic point of view, if we can reduce the levels of Zeb1 in diabetic patients, then we may be able to achieve healthy blood vessel growth in wounds. First, we need to do more preclinical research before we can go clinical.
What are the next steps for this research?
Now we are going to look into more mechanisms that detail how Zeb1 in hyperglycemia is a pathogenic for endothelial cells. Then we can come up with some molecular targets or drugs that can reduce Zeb1 levels in diabetic wounds.
