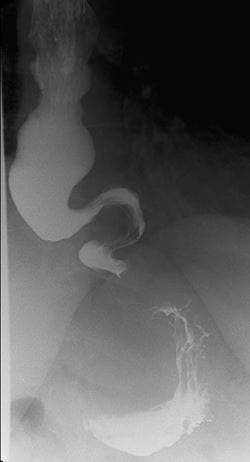
Indiana University School of Medicine faculty physicians are the exclusive gastrointestinal (GI) and hepatology care providers at IU Health University Hospital, Eskenazi Health and the Richard L. Roudebush VA Medical Center in Indianapolis. Faculty experts treat swallowing disorders, eosinophilic esophagitis, peroral endoscopic myotomy (POEM) for achalasia and gastroparesis, gastric electrical stimulation for gastroparesis, small bowel motility disorder, small intestinal bacterial overgrowth (SIBO), constipation and fecal incontinence.
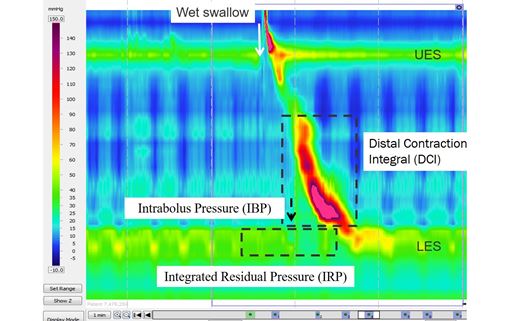
The GI Motility laboratory offers state-of-the-art diagnostic testing of the upper and lower GI tract, such as high-resolution esophageal manometry, pH-impedance monitoring, wireless Bravo pH testing, electrogastrography (EGG), endoFLIP distensibility testing of esophagus and pylorus, antroduodenal manometry, anorectal manometry/compliance and hydrogen breath test for SIBO and carbohydrate malabsorption. The GI Motility lab performed over 2,000 procedures in 2019.